
Tick-borne borreliosis (aka Lyme disease) is the second most important tick-borne infection after tick-borne encephalitis in Eurasia. Only in Russia, 3-3.5 times more cases of human infection with it are registered annually than cases of infection with tick-borne encephalitis.
In some regions, Lyme borreliosis is generally the only epidemiologically significant infection transmitted ixodid ticks. And only the relative ease of treatment and the lower lethality of this disease make it possible to consider it less formidable than tick-borne encephalitis.
However, tick-borne borreliosis is very dangerous. In its neglected form, without competent treatment, it can lead to severe disability and death of the patient, and with incorrect or delayed treatment, it can turn into a chronic form or cause incurable complications that significantly reduce the quality of human life.
At the same time, Lyme disease is very variable - both in symptoms and in clinical manifestations. Often it can be difficult to diagnose, and in some cases, borreliosis "mimics" less serious diseases that at first do not cause concern to the patient. Sometimes the infection does not manifest itself clinically at all, but at the same time causes complications, which themselves can cause the patient to become disabled.

All this shows how important tick bite timely diagnosis and correct treatment of tick-borne borreliosis. Moreover, even taking into account the wide variety of symptoms and forms of the course of this disease, it is quite possible to detect and cure it in time even before the development of dangerous complications and a threat to the life of the patient.
Basic information about tick-borne borreliosis
Tick-borne borreliosis is a bacterial disease. It is distributed circumpolar in the Northern Hemisphere, that is, the area in which it is more common covers the globe with a ring broken by only two oceans. At the same time, the largest number of diagnosed cases of the disease was noted in the United States, Canada and Russia, and significantly less in Western European countries.
On a note
Borrelia genes were found in the remains of a person who froze in the Alps more than 5,000 years ago - there is reason to believe that the disease "hosted" the heart of Europe long before it was first discovered in the United States (in 1977).
For the first time, borreliosis, as an independent disease, began to be discussed in the late 70s of the last century in the United States when clinically similar arthritis of unknown origin was found in many children.

Blood tests made it possible to identify, first, antibodies to Borrelia, and then the pathogens themselves. Even later, the cycle of development and transfer of these pathogens by means of ticks from one host to another was completely deciphered.
The name of the disease comes from the name of the city of Old Lyme, in which similar cases of arthritis in children were first documented.. In the course of studying the pathogenesis of the disease, it was possible to establish its connection with tick bites and the appearance of a characteristic annular migratory erythema. The ICD-10 disease code is A69.
The photo below shows what characteristic erythema annulare looks like at the site of the bite. borreliosis tick:

After the development of effective diagnostic methods, the epidemiological picture became clearer, and it became obvious that tick-borne borreliosis is not at all a rare disease. For example, in 2011, 9957 cases of the disease with 34 deaths were registered in Russia alone, in 2016 - 6103 cases and 30 deaths.
On a note
For comparison: tick-borne encephalitis in 2011 was registered in 3527 patients, in 2016 - in 2035 people.
Lyme disease can develop in many vertebrates, and humans are not its main natural reservoir. Given the relative ease of treatment and the extremely low chance of the pathogen being transmitted from person to another host, humans can be considered a kind of "dead end" branch in the spread of Borrelia. In the greatest quantities, borreliosis affects birds (especially passerines), rodents, wild ungulates and livestock, as well as canines - wolves, foxes, raccoon and domestic dogs.
Tick-borne borreliosis is carried only by ticks. It is impossible to get infected by contact with a sick animal or person, including, for example, by a dog bite. That is why the area of the disease is strictly limited to habitats. tick species, which are carriers of Borrelia, as well as the range of their owners in the warm season of the year, when ticks attack them.

From the point of view of the mechanism of development, both in animals and in humans, borreliosis proceeds similarly, although its external signs can vary significantly.
Lyme borreliosis is very variable in the forms of its course.Its incubation period can range from 2 days to several years, the disease can be acute, chronic and asymptomatic, the clinical picture can be blurred and atypical, and the symptoms themselves are mostly nonspecific and do not accurately indicate the disease.
An unambiguous sign of infection - ring migrating erythema - does not always develop, and it is quite difficult to detect the causative agent of the disease directly in the blood or tissues. For an accurate diagnosis of the disease, a blood test for antibodies to the pathogen is required.
Treatment of borreliosis with timely onset is relatively uncomplicated, inexpensive antibiotics are available for it. But measures of specific prevention of the disease are not practiced, that is, antibiotics are not used “just in case” - they are prescribed only when the development of the infection is confirmed.
To make a short summary: tick-borne borreliosis is widespread, dangerous (if not treated), difficult to diagnose and prevent, but with timely access to a doctor, it is relatively easy to treat.
The causative agent of the disease and its relationship with ixodid ticks
Tick-borne borreliosis is caused by spirochetes from the genus Borrelia. To date, at least 6 species of Borrelia are known, infection of a person with which leads to the development of borreliosis. The most common of these is Borrelia burgdorferi, which is responsible for the largest number of cases.
The photo below shows what Borrelia burgdorferi looks like under a microscope:
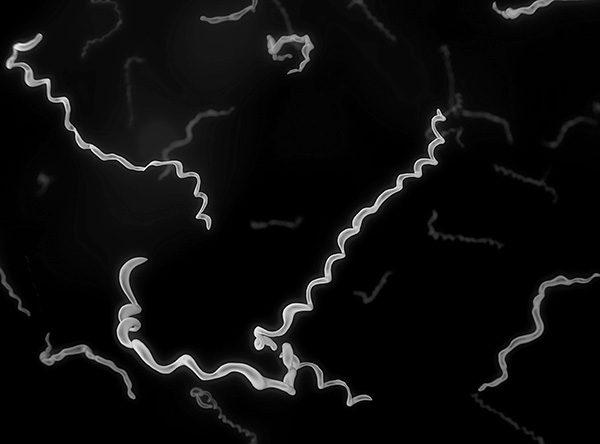
Borrelia burgdorferi is the causative agent of tick-borne borreliosis.
Other types of borrelias dominate as causative agents of borreliosis in Europe and Asia. It:
- Borrelia garinii;
- Borrelia miyamotoi;
- Borrelia spielmanii;
- Borrelia afzelii;
- Borrelia bavariensis.
In clinical practice, all these species are often referred to as Borrelia burgdorferi s. l., that is, "in the broadest sense." The fact is that the exact identification of the type of bacteria is quite difficult, and such identification is not required for the successful treatment of the disease. For diagnosis, it is enough to find out that the pathogen belongs to the genus Borrelia, and for simplicity it is referred to the most common species (burgdorferi). Species identification is carried out mainly for scientific and research purposes.
Throughout the distribution area, Borrelia parasitize in many vertebrate animals: birds, dogs, rodents, and cattle. Due to this versatility, they can easily spread with their owners to new areas, but so far they have not been found in the Southern Hemisphere.
On a note
For domestic dogs, the disease is as dangerous as for humans, and requires emergency treatment.
Photograph of annular erythema migrans on a dog's body:

The causative agents of borreliosis are closely related in their biology to ixodid ticks. The fact is that borrelia are not able to move from one host to another without the participation of a tick, and therefore, when an infected animal (or person) dies, they also die. The only way to transfer them between hosts is to enter the tick's digestive tract with blood, infect its body, develop and reproduce, and then infect (with the tick's saliva) a new victim.
On a note
In different types of ticks, the state of the body changes differently when infected with Borrelia. Thus, in the American Ixodes pacificus, infected females lay significantly fewer eggs than healthy ones.And in the black-footed tick, infected nymphs are distinguished by greater survival and life expectancy than uninfected ones (at the same time, adult infected ticks, on the contrary, turn out to be less viable). At taiga tick (Ixodes persulcatus) there were no changes in condition and viability when infected with Borrelia.
Thus, it is possible to become infected with borreliosis only from a tick. It is impossible to get infected from a sick person or animal while caring for him or through direct contact.
On a note
It is believed that when a pregnant woman is infected with borreliosis, vertical transmission of the infection and infection of the fetus is possible. However, there are no documented cases of congenital borreliosis in newborns. The hypothetical possibility of infection of the fetus is the basis for intensive antibiotic therapy of pregnant women with borreliosis.
As a rule, the primary entry of Borrelia into the body of a tick occurs at the nymph stage. Then borrelia safely survive the molting of the parasite, migrate to the salivary glands, and when an adult tick feeds, they enter the body of a new host.

In the body of the tick, Borrelia colonize almost all tissues, but multiply in the largest quantities in the digestive tract. In this they differ from many other pathogens of tick-borne infections, which are not able to stay in the intestines of the parasite for a long time and quickly move to other tissues.
As a result, when a parasite bites, the rate of transmission of infection to a person is low, since there are not so many borrelia in the salivary glands of the tick, and the pathogen from the tick’s intestines into the human blood is very unlikely (see also the article How a tick bites: details about the process when it digs into the skin). This means that if the tick is removed immediately after sucking, then even if it is infected with borreliosis, it is possible to avoid infection with Lyme borreliosis with a high probability.
Transmission of the pathogen from a tick to a person
Human infection with Borrelia occurs when the tick feeds. After the parasite bites through the skin, it injects into the subcutaneous tissue saliva containing blood anticoagulants, anesthetics, lysing components, sometimes (in some species) cementing compounds, and some other substances.
If a tick has already developed a borreliosis infection in the body and the borreliae have managed to penetrate into the salivary glands, then the transmission of pathogens is possible already at the first injection of saliva into the bite site.
If the parasite is not removed, then it will feed on a person from 2 to 5 days. During this time, with a frequency of 15 minutes to 2-3 hours, the tick regularly introduces new portions of saliva into the wound, then sucks out a portion of blood, after which it pauses and rests. It is at the moment of saliva injection that infection occurs.

With a single injection of saliva, a relatively small number of borrelia are transmitted under the skin - from a few units to several hundred. This is less than the minimum infectious dose, since the probability that at least one of these borrelia will escape destruction by the components of nonspecific immunity and survive in a new organism is very small. Therefore, as noted above, if the infected tick is removed immediately after sucking, the infection can be avoided with a high probability.
There are no clear deadlines here - a heavily infected adult female can introduce an infectious dose of the pathogen into the body already in the first half hour after the bite, and a small nymph can have time to feed 60 minutes before it is detected and removed, but will not transmit a significant amount of borrelia, and a person will not become infected.
On a note
According to statistics, the probability of getting sick with tick-borne borreliosis when bitten by a tick in Russia in epidemiologically disadvantaged regions for this disease ranges from 1.3-1.8%. That is, for 1000 people bitten by ticks in general (both infected and not infected), 13-18 people fall ill with borreliosis.
This means that if a tick is found on the body, it must be removed as soon as possible., even at the risk of tearing the head off the body for lack of hand special device for removing ticks. If the mouthparts of the parasite remain in the skin, they will no longer lead to infection, since the salivary glands will be removed. And the remnants of the tick in the skin can be easily removed with a needle or tweezers - like a regular splinter.

Conclusion: if a stuck tick is found on the body, and there are no tools at hand to remove it, the parasite must still be removed, even with your fingers, but in no case should you wait an extra couple of hours until it becomes possible to remove it “according to the rules” or visit a doctor.
In this regard, see also the article First aid for a tick bite in humans.
On a note
Borreliosis is not transmitted directly from person to person. From the patient can not be infected through household contact, kissing or sexual intercourse.
Development of the disease
When a tick bites a person, borrelia enter the subcutaneous tissue with the saliva of the parasite, in which inflammation already occurs.
The inflammatory exudate that accumulates here as a result of the reaction of the immune system to tick-borne antigens is also one of the components of the bloodsucker's food, and the bacteria, in fact, enter the "broth" from the blood, lymph and the remains of destroyed cells. They are immediately attacked by macrophages that migrated here when inflammation factors appeared - some of the bacteria die, some cannot reach the cells and go beyond the inflammation zone (as a result, some of them are sucked back by the tick).
And only a small part of Borrelia reaches healthy cells surrounding the area of inflammation, and is introduced into the intercellular spaces between them. Here they begin to actively multiply, spread through the fiber, and eventually penetrate into the blood and lymph, with which they spread throughout the body.

Depending on the damage to certain organs, various signs of the disease develop, allowing it to be divided into several stages:
- At the first stage, Borrelia actively multiply in the skin near the bite site, but do not yet affect the internal organs of a person. The stage begins immediately after the completion of the incubation period, which can last from 2-3 days to several months (rarely up to 2-3 years). It is characterized by the appearance of migrating erythema, which clearly indicates where borrelia accumulate under the skin: there are practically none in the center of the ring, but on the periphery, in places of greatest redness, the concentration of infectious agents is highest. At this time, many bacteria begin to die, releasing toxins. It is these toxins that cause fever - fever, nausea, muscle aches, malaise, headaches.This combination of symptoms is nonspecific and does not unequivocally indicate borreliosis, which is why, in the absence of erythema, the disease is often mistaken for a common ARVI. The first stage of tick-borne borreliosis lasts from 3 to 32 days, then either recovery occurs or the disease passes into the second stage (usually with a short pause, during which the patient feels well). With adequate treatment at the initial stage, the disease is cured completely and leaves no complications;
- The second stage of borreliosis begins 1-3 months after the tick bite and is characterized by active dissemination of the pathogen in the body with damage to various internal organs and systems, primarily nervous and cardiovascular. Systemic borreliosis develops (a generalized form of borreliosis). It is accompanied by meningitis, nervous disorders, heart damage. Without treatment at this stage, the disease can become chronic and cause complications that are difficult to treat. Without treatment, the disease can cause tonsillitis, bronchitis, conjunctivitis, hepatitis, choriretinitis and other inflammatory diseases;
- The disease passes into the third stage after a long period from the moment of infection - usually from six months to 2 years. At this stage, the joints suffer greatly, lesions of the skin and nervous system develop (the latter resemble the clinical picture of neurosyphilis).
In the absence of treatment at the end of the third stage, the disease can become chronic. In this case, both alternating relapses with remissions and a continuous sluggish relapse with aggravated arthritis, sometimes complicated by osteoporosis with severe destruction of bones and cartilage, can develop.Damage to the nervous system or heart at this stage can cause death.
The photo below shows the deformity of the leg due to arthritis that developed against the background of Lyme borreliosis:

On a note
Mortality from tick-borne borreliosis averages about 0.3-0.35%, that is, out of 10,000 infected, 30-35 people die from this disease or the complications it causes. In Russia, for the period from 2011 to 2016, 176 cases of death of people from Lyme disease were recorded.
Lesions of certain organs proceed according to the usual inflammatory type. That is, it is impossible to understand from external symptoms alone that, for example, meningitis or arthritis is caused precisely by borreliosis. This complicates the diagnosis of Lyme disease.
Symptoms and clinical picture at different stages of the development of the disease
Diagnosis of tick-borne borreliosis is difficult due to the wide variety of symptoms and forms of this disease.
The most characteristic, easily diagnosed and common symptom of the disease is erythema migrans annulare. It develops around the site of the tick bite, first as a simple redness, which increases in size over time, and disappears directly at the site of the bite. A well-marked red ring is formed. The photos below show a few examples:


The appearance of annular erythema clearly indicates infection with tick-borne borreliosis. If correct treatment is started at this time, then all serious consequences can be avoided.
However, erythema migrans annulare develops in only 60-80% of infected people. In the rest, it is necessary to diagnose borreliosis on other grounds.
So, at the first stage, the disease usually manifests itself as a typical febrile syndrome characteristic of SARS.The patient's body temperature rises, nausea, malaise, pain in the muscles and head appear. This condition lasts, as a rule, a week and a half, then passes.
In the second stage of the disease, various signs of damage to the nervous system may appear:
- Paresis of cranial nerves;
- Throbbing pain in the temples;
- Photophobia;
- Fast fatiguability;
- Chorea.
Children often show signs of damage to the meninges and brain, in adults - damage to the peripheral nervous system.
Somewhat less often, signs of heart damage are manifested: conduction disturbance according to the blockade type, myocarditis, pericarditis, severe squeezing pains in the chest. Even more rare symptoms are hepatitis, conjunctivitis, bronchitis and, in fact, inflammatory diseases of any internal organs.
In the second stage of the disease, benign lymphocytoma of the skin can develop - another specific sign of Lyme disease. This neoplasm consists almost exclusively of lymphocytes and histiocytes, does not pose a health hazard, but looks unaesthetic. Its appearance in the absence of other signs of borreliosis indicates an asymptomatic course of the disease.
The photo shows such a benign lymphocytoma:

Relatively rarely, both the first and second stages of borreliosis are asymptomatic, and the disease manifests itself only when the joints are affected. In these cases, the only way to diagnose tick-borne borreliosis is to take a blood test specifically for this infection.
Practical points: how to track the onset of the disease and detect infection in time
In view of the foregoing, the main difficulty in diagnosing Lyme borreliosis is that without the appearance of migrating erythema (that is, in about every third case), the patient does not suspect at all that he is developing this particular disease. Consequently, he either does not take measures for treatment at all, or these measures turn out to be incorrect (for example, a person begins to treat a “cold”).

In order to detect infection with borreliosis in time, you should:
- Remember (or better write down) the date of the tick bite. If a tick has bitten a child, this must be done by parents;
- If ring migrating erythema or lymphocytoma appears, immediately contact the clinic to clarify the diagnosis;
- If any generalized symptoms appear within 2-6 months after a tick bite, consult a doctor and inform him about the recent bite. After that, donate blood for analysis for tick-borne infections;
- If generalized symptoms do not appear within six months after the bite, it is useful to simply donate blood for testing for borreliosis. In rare cases of asymptomatic disease, this is the only way to detect it.
It is the blood test for borreliosis that is the most representative study. According to its results, specific antibodies to Borrelia are detected in the blood, the composition of which allows us to assess, among other things, the approximate stage of the course of the disease. In this case, blood is donated not earlier than the end of the incubation period. A positive result in this case is highly likely to indicate an active infection.
A less effective way is to study tissues and whole blood in order to detect Borrelia DNA by PCR.The fact is that these pathogens themselves are very small, and distributed in tissues with a low density, and therefore it is not always possible to find them in sufficient concentration, even if they are present here. For such tests, skin fragments (usually from an erythematous area), blood, urine, and synovial fluid from affected joints may be examined.
Finally, it is not always advisable to examine the tick itself for infection with Lyme borreliosis. Even if the parasite turned out to be infected with Borrelia, this does not mean at all that human infection certainly occurred during its bite - that is, uncertainty will still remain.
How is Lyme borreliosis treated?
The basis of the treatment of borreliosis is antibiotic therapy with the use of drugs to which borrelias are sensitive. With correct and timely treatment, it is possible to avoid the development of neurological and cardiological complications, as well as damage to the joints. With therapy at later stages, treatment greatly alleviates the patient's condition and prevents the chronicity of the disease, however, individual disorders in the body can persist for life.
Antibiotics of the first line of choice are tetracyclines, usually tetracycline itself, less often doxycycline, glycocycline. The drug is used for 10-14 days, and the death of the main number of bacteria occurs already in the first few days of therapy. A full course is necessary for the complete elimination of the pathogen and reliable prevention of complications.

On a note
If tetracyclines are unavailable or ineffective, the patient may be prescribed penicillins (benzylpenicillin, amoxicillin, ampicillin) or cephalosporins (ceftriaxone, cefotaxime, and others).
In parallel with antibiotics, if necessary, patients are given symptomatic therapy, the purpose of which is to alleviate the patient's condition. To do this, use anti-inflammatory, anticonvulsant, detoxification, analgesic, dehydration agents - depending on the symptomatic picture.
Treatment is usually carried out on an outpatient basis, with regular visits to the doctor, who gives the necessary clinical advice.
Some complications of borreliosis require much more complex and lengthy treatment than the disease itself. For example, with developed arthritis, it is often necessary to treat the patient for a long time, and without a guarantee of a complete cure. With the development of atrioventricular blockade, it may be necessary to perform a heart operation.
In general, the prognosis for tick-borne borreliosis largely depends on the stage of the disease at which intensive therapy began. With the timely start of treatment, the disease, as a rule, ends without consequences. In the second and third stages, it is possible to achieve complete elimination of the pathogen while maintaining certain complications (usually on the joints, less often - neurological and cardiological). In some cases, the developed complications are not subject to a complete cure.
Available ways to prevent the disease
To date, there are no means and methods for the specific prevention of tick-borne borreliosis. A vaccine against this disease has not been developed and is unlikely to be developed, since even acute borreliosis does not leave behind stable immunity, and a few years after its cure, re-infection is possible.

Also, measures for emergency prevention of borreliosis are not practiced - in contrast, for example, from tick-borne encephalitis (it is considered inappropriate to prescribe rather heavy antibiotics to a person bitten by a tick without confirming the disease).
It is absolutely impossible to take antibiotics on your own (on your own initiative) simply because of a tick bite.
So the most effective way to protect against borreliosis today is to reduce the likelihood of a tick bite. Read more about this in the article How to protect yourself from ticks in nature.
On a note
According to the requirements of SanPin, for the prevention of borreliosis and tick-borne encephalitis, public spaces - parks, squares, playgrounds in kindergartens - should be regularly treated with acaricidal preparations. Nevertheless, given the fundamental impossibility of treating all grass-covered areas in the city, it is impossible to be sure that there are no ticks here. In addition, judging by the reviews, ticks are often removed from dogs and people even after walking through areas treated 1-2 months ago.
Considering that dogs also suffer from borreliosis, it is advisable for them to use special drops on the withers, sprays or anti-flea collars.
If you have personal experience in the treatment of tick-borne borreliosis, be sure to share the information by leaving your feedback at the bottom of this page (in the comment box).
The danger of tick-borne borreliosis for humans



