One of the main tasks of a person after a tick bite is to carefully monitor their own condition in order to be able to detect the symptoms of a disease that could have been infected by a bite. Ticks are able to carry many infections (not only the causative agents of tick-borne encephalitis and borreliosis), and the diseases caused by such pathogens can lead to irreversible disability and even death of a bitten person.
By itself, the bite of the parasite is practically harmless, and if the infection does not occur, then the itchy bump that develops in its place quickly and without consequences disappears (as happens after mosquito bites).

Next, we will talk about exactly how the symptoms of infection appear after a tick bite, how long it takes and, most importantly, how to act in a given situation. And also let's see by what signs it is possible to understand that it was the tick that bit, and not some other parasite.
What infections can you get from a tick bite?
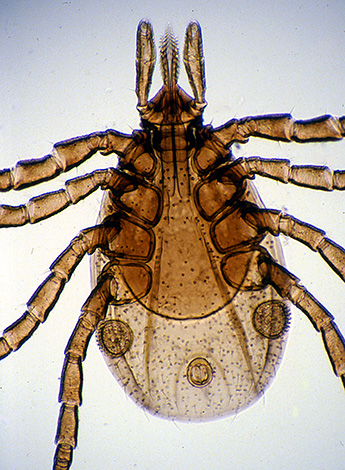
ixodid ticks - the very ones that bite humans most often in Eurasia - are carriers of more than 350 types of various pathogens that are dangerous to humans and domestic animals. More than 100 types of viruses, more than 200 types of piroplasmids, 30-35 types of rickettsia and several types of trypanosomes, bacteria, filariae and spirochetes were found in the parasite organism.

However, many of these pathogens are not dangerous to humans, and are species-specific only for some animals. For example, piroplasms cause a deadly disease in dogs (piroplasmosis), but are not dangerous to humans.
In addition, some of the pathogens carried by ticks are very rare and cause disease in humans in isolated cases. They are not considered as epidemiologically significant pathogens.
As a result, in the territory of Eurasia, only two tick-borne infections are epidemiologically significant and pose a real threat to human health and life:
- Tick-borne encephalitis (ICD code 10 - A84) is a disease caused by the tick-borne encephalitis virus and leading to lesions of the brain and meninges. Without proper treatment, it can lead to lifelong mental impairment and death;
- Lyme borreliosis (aka Lyme disease, ICD-10 code - A69.2) is a bacterial infection with a wide variety of clinical forms. It can be asymptomatic, it can be chronic, it can develop rapidly and also end with the disability of the patient, or with the development of complications that reduce the quality and life expectancy (for example, with lesions of the heart or joints). A fatal outcome is also possible.
Both diseases are distributed throughout Eurasia, although very unevenly. For example, tick-borne encephalitis is most often recorded in Eastern Siberia and eastern Kazakhstan, the Northern Urals and the Far East.Previously, endemic outbreaks of it regularly occurred in Central Europe, but today encephalitis is recorded there less and less, largely due to state vaccination programs for the population living in epidemiologically dangerous regions.
In the south of Russia, in Ukraine, in western Kazakhstan, tick-borne encephalitis is rare, and in some areas it does not occur at all.
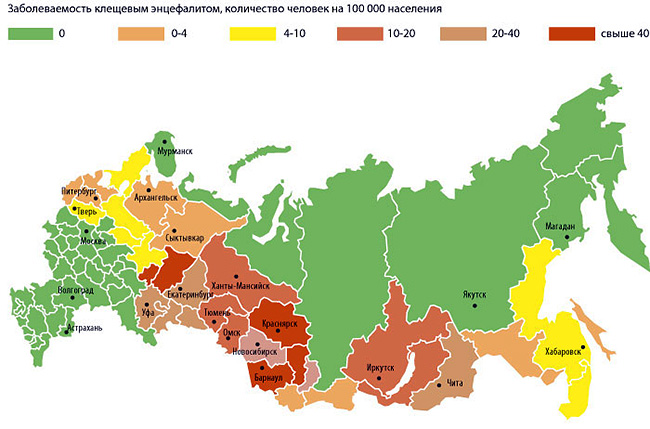
Borreliosis, on the contrary, is more common in Europe and the western part of Russia.
On a note
The chance of infection from a single tick bite is very low. Thus, according to statistics, only 6% of ticks in epidemiologically dangerous regions are infected with the tick-borne encephalitis virus. Out of 100 cases of bites by infected ticks, the disease develops in about 3-5% of people. Therefore, the probability of infection in a dangerous region is only about 0.24%. That is, for a thousand bites, there are less than 3 cases of the disease.
In borreliosis, this indicator is also low, and therefore, if one tick is found on the body and it is quickly removed, the probability of the disease will be very small. People who are in the wild for a long time, who are sucked by several ticks at the same time and who do not have the opportunity to regularly examine the body and quickly remove parasites, are at serious risk.

It is noteworthy that one tick can be a carrier of both tick-borne encephalitis virus and Borrelia at the same time. Therefore, when bitten, it is possible to become infected with a mixed infection with a “double” danger to humans. However, this happens extremely rarely.
It is important to understand that ticks transmit infectious agents only when they bite, when inject saliva into the wound. If the tick only crawled through the body, but did not stick, infection will not occur.At the same time, tick-borne encephalitis can be contracted by eating fresh milk of goats that carry the virus. Symptoms of TBE in this case will be the same as with a parasite bite.
What are the dangers of these diseases and how they proceed
Both tick-borne encephalitis and Lyme disease are most dangerous due to the involvement of nervous tissue in the pathological process, which leads, among other things, to irreversible disorders. Patients can develop nervous pathologies, dementia, memory loss, paralysis, and without proper treatment, these consequences become irreversible, leading to disability. In especially severe cases, both tick-borne encephalitis and Lyme borreliosis end in the death of a person.

However, pathogenetically and clinically, these diseases differ significantly.
So, with tick-borne encephalitis, the cells of the nervous system become the targets of viral particles. The disease develops rapidly, its symptoms are rapidly increasing both quantitatively and in their severity. In some cases, CE develops so quickly that the patient does not even have time to be taken to the hospital.
Chronic forms of tick-borne encephalitis are not known. The disease is either cured with the formation of neurological insufficiency (disability with mental disorders) or without it, or ends with the death of the patient. When infected with a virus of the European subtype, mortality is 1-2%, when infected with a virus of the Far Eastern subtype - 21-24%. In this case, death usually occurs 5-7 days after the development of the first neurological symptoms.
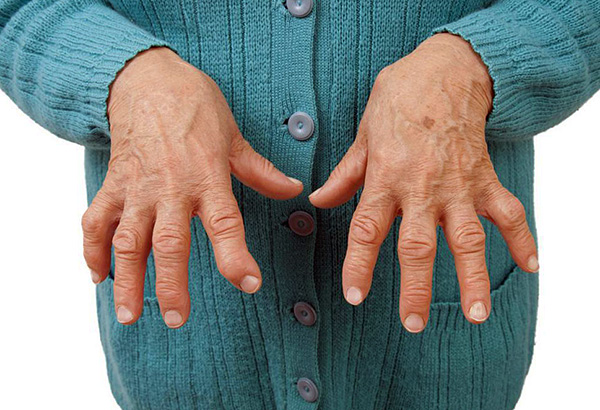
Almost every organ and tissue in the body can be affected in Lyme disease. In advanced cases, the disease leads to arthritis, hepatitis, damage to the heart muscle, brain, organs of vision and hearing.When a pregnant woman is infected, vertical transmission of the pathogen to the fetus can occur with the development of congenital borreliosis.
In most cases, untreated borreliosis becomes chronic with the development of numerous complications. Deaths after it, if recorded, are months after the onset of the disease (mainly from complications).
Treatment options also differ. Tick-borne encephalitis, as a viral disease, is not treated specifically, that is, there is no such medicine that would kill the TBE virus particles. For its treatment, blood sera with immunoglobulins, immunomodulators, interferon preparations, and agents to relieve severe symptoms are used. In general, therapy is complex and not always completely effective.
Borreliosis is easier to treat. Its pathogens are sensitive to available and inexpensive antibiotics, and if treatment is started on time, the disease is quickly cured. Today, methods of treating advanced forms of borreliosis have even been worked out, but with them there is a possibility of residual disorders remaining after a complete cure. In particular, the development of arthritis, chronic heart damage and neurological disorders associated with autoimmune mechanisms that are difficult to correct is possible during treatment in the later stages.
Obviously, the sooner the symptoms of a tick infection are detected, the sooner treatment can begin. This means that the greater the likelihood of a successful outcome without irreversible consequences.
Now let's see when, after a tick bite, wait for the first symptoms of the disease to appear ...
When can the first signs of infection appear after a tick bite?
The first clinical symptoms indicate the completion of the incubation period of the disease. When infected with tick-borne encephalitis, such symptoms appear after 7-12 days, similarly for Lyme disease, however, borreliosis in this respect is much more variable.
On a note
There are known cases of the appearance of the first symptoms of borreliosis already 2-3 days after the removal of the tick (which may be due to the prolonged suction of the parasite, when the infection occurred on the first day of the bite, the tick was removed on 3-4 days, and after another 2 days signs of infection appeared) . There are also cases of manifestation of Lyme disease several months and even 1-2 years after the bite.
To some extent duration of the incubation period for tick-borne encephalitis depends on the subtype of the virus and the health of the bitten person. Encephalitis of the Far Eastern subtype usually develops faster, and its symptoms appear earlier - 6-7 days after the bite. The manifestation of signs of infection on days 12-14 is typical mainly for the Western European subtype.
In people who have not been bitten by ticks before, the disease usually develops faster than in those who have already encountered ticks. This is due to the fact that even without specific immunity to the TBE virus, the body after a tick bite produces antibodies to the components of its saliva. In the future, it is these antibodies that will provide a rapid immune response to the entry of parasite saliva components into soft tissues and slow down the infection of the body.

Lyme borreliosis is characterized by the same dependence, but less pronounced. Immunity to its pathogen persists for several years.
Also, the rate of development of symptoms of the disease depends on how long the tick sucked blood. Usually the parasite sticks for several days, and sucks blood not constantly, but intermittently. With the same intervals, he injects saliva with infectious agents into the wound. The more acts of salivation the parasite managed to perform, the more pathogens will enter the bloodstream. And consequently, other things being equal, the faster the disease will develop in the human body and the faster its clinical signs will appear.
It is interesting
The causative agent of tick-borne encephalitis accumulates in large quantities precisely in the salivary glands of the tick, and therefore, when bloodsucking, it is transmitted relatively quickly. Borrelia, on the other hand, mainly inhabit the digestive tract of the parasite, and are found in small numbers in the salivary glands. That is why the probability of infection with borreliosis is relatively small, despite the large number borreliosis ticks, which are its carrier.
In some cases, Lyme borreliosis can occur in an erased, asymptomatic form. This situation is especially dangerous, since a person does not notice the signs of the disease, but the infection itself in the body develops and affects various tissues and organs. Then, much later, complications may appear that are not always amenable to therapy. That is why it is advisable to take blood tests for borreliosis some time after a tick bite.
Is it possible to understand by the appearance of the bite or the parasite itself that an infection has occurred?
Directly at the bite, immediately after it, or even the next day, it is impossible to determine by any visual signs or sensations that the biting tick was infected with an infection and could transmit it by bloodsucking.
For details, see the article How to distinguish an encephalitic tick from a common (non-infectious) parasite.

Ticks, whose salivary glands and digestive tract contain pathogens of infectious diseases, outwardly do not differ from uninfected parasites. Their behavior is also completely identical to the behavior of pathogen-free brethren.
On a note
The tick-borne encephalitis virus and Borrelia do not pose a threat to the bloodsucker itself and practically do not affect his life.
By the appearance of the bite mark, in most cases it is also impossible to say for sure whether a person has become infected or not.
But to distinguish a tick bite from the bite of any other blood-sucking or stinging arthropod is very simple. The tick never bites quickly and never tries to hide immediately after piercing the skin. Its task is to feed on blood, and the nutrition itself usually lasts several days, but not less than 10-15 hours. Therefore, almost always at the site of the bite, the attached tick itself is found. If it is not there, then someone else has bitten it.
Exceptions to this rule are relatively rare, but possible. For example:
- A person has previously been repeatedly bitten by ticks and his body has developed an immune response to tick-borne antigens. Sometimes this response is so powerful that the tick cannot fully suck blood due to the neutralization of its own enzymes. In such a situation, the parasite can detach within 40-90 minutes after attachment, and only a small puncture of the skin and slight swelling will be found at the site of the bite.;
- A person rarely examines himself, or does not do it at all. In such a situation, the tick can calmly suck blood for 3-4 days, and then detach itself, leaving a small wound and swelling at the site of the bite. It will be difficult to accurately identify the parasite from this trail;
- There are times when a child finds a tick on himself, tears it off, but does not tell his parents.
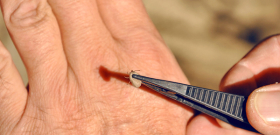
The photo below shows a typical ixodid tick bite:

In all these cases, redness 1-3 cm in diameter remains at the site of attachment of the parasite, the skin is dense, with a clearly visible dark skin puncture site in the middle. In some people, a bump forms, it itches severely during the first days after detaching or removing the tick, and when combing, the itching intensifies.
On a note
According to ICD-10, a tick bite is assigned the code W57 - "Bite or sting by non-poisonous insects or other non-poisonous arthropods."

From the bites of stinging insects, which often occur in nature, tick bites are distinguished by the absence of sharp pain. They are easily distinguished from mosquito bites by the presence of a dark dot at the site of the skin puncture. But the bites of midges, biting midges, some flies can be very similar to them, but, again, detecting a tick bite without the parasite itself in the skin is a rarity.
It is impossible to immediately feel and by some sensations understand that the tick has stuck to the body. The bite occurs painlessly and imperceptibly, and therefore it is possible to find out that, for example, a bloodsucker has stuck into the skin on the head in the hair or in the groin only when examining the body.It is easy to recognize the parasite - its body sticks out of the skin like condyloma, and if the parasite is large, then it is easily evident. On the contrary, it is not easy to detect small nymphs even on smooth areas of the skin, so you need to carefully examine the whole body, especially the groin, armpits, skin between the fingers, neck.
On a note
Directly under the skin or into various cavities of the body - deep into the nose, into the ears - ticks do not climb. Accordingly, they do not live here and do not cause corresponding pathologies.
The first symptoms of tick-borne encephalitis
The earliest symptoms of tick-borne encephalitis are nonspecific and do not allow a person to confidently distinguish it from many other infectious diseases.
So, at the end of the incubation period appear:
- Typical febrile syndrome with fever, malaise, pain in the muscles and in the head;
- sleep disorders;
- Loss of appetite.
With encephalitis of the European subtype, such a fever can last 2-3 days, and then passes, and the person believes that these were some kind of mild form of SARS. However, after a week of remission, the second, meningeal or encephalitic phase begins with damage to the membranes of the brain and spinal cord and the development of neurological symptoms, which include:
- inability to turn the neck;
- Severe throbbing headaches;
- Loss of consciousness;
- convulsions;
- Paralysis;
- Violations of the sensitivity of the skin.
These symptoms are accompanied by fever, usually more severe than in the first phase. Over time, they intensify and, if left untreated, often lead to the death of the patient.
Encephalitis of the Far Eastern subtype proceeds without remissions and division into phases.At the end of the incubation period, fever develops, often with a sharp jump in temperature to 38-39 ° C. On the third or fourth day, symptoms of damage to the nervous tissue appear, they quickly increase, and on the 4th-5th day, if left untreated, death occurs.
Encephalitis of the Siberian subtype is clinically similar to the Far East, but may develop somewhat more slowly. With it, recovery occurs more often even in the absence of treatment (sometimes with residual health disorders).
Lyme borreliosis symptoms
Symptoms of Lyme borreliosis in most cases are also non-specific: the disease begins with fever, malaise and muscle pain, which can be mistaken for SARS or signs of food poisoning. Sometimes, already at an early stage, this set is supplemented by the stiffness of the muscles of the neck - a person has to turn the entire upper body to look sideways.

Perhaps the most definitive sign of Lyme disease is erythema migrans annulare, a prominent red ring on the skin around the bite site. It develops in 65-80% of patients and sometimes appears earlier than fever. Its development is very characteristic: redness at the site of the bite gradually expands to neighboring tissues, a large spot forms, until a ring of normal skin color suddenly appears around the bump itself. The photo shows what it looks like:

This ring can grow up to 20-25 cm in diameter, the skin at the site of redness can itch, peel off, sometimes even die.

In some people, the same erythema appears on other parts of the body where there are no bites - they are associated with an allergic reaction of the body to the pathogen and its antigens.

Ring erythema keeps on the skin for several weeks, sometimes - until the end of the disease. Sometimes it may not be visible if it is, for example, on the back, and therefore another person should check the bite site.
A few days after the first symptoms of borreliosis appear, other specific signs may appear:
- Conjunctivitis;
- Photophobia;
- Hepatitis;
- Hives.
After about a month, these symptoms are joined by manifestations of meningitis and lesions of internal organs: facial muscle paresis, memory lapses, joint pain, chorea. Even later, if treatment has not been started, arthritis, bursitis, atrophic acrodermatitis and other syndromes develop.
In some cases, the first phases of the disease are asymptomatic, and severe lesions develop unexpectedly. As a result, a person with borreliosis does not see the connection between these symptoms and a tick bite, does not inform the doctor about it, and he cannot make a correct diagnosis.
All this means that any signs of illness within 2-3 months after a tick bite should be monitored, and if they appear, report them and the bite itself to the doctor. Even if no signs of the disease have appeared, 2-3 weeks after the bite of the parasite, it makes sense to take a blood test for borreliosis.
First steps to take when symptoms appear
With the likelihood of developing borreliosis and tick-borne encephalitis, it is unacceptable to rely on self-diagnosis, and even more so - on treatment at home.If you feel any discomfort after a tick bite (as well as when erythema migrans appears), you should consult a doctor as soon as possible. An initial consultation can be obtained from a therapist, and he will already refer the patient to an infectious disease specialist.
When the first symptoms of the disease appear, all tests that are carried out in such cases will be indicative. If encephalitis is suspected, the patient may be referred for an immunological analysis and a complete blood count. So, already on the 3rd-4th day of illness, acute-phase immunoglobulins of class M (IgM) are detected in the blood, confirming the development of TBE.

A general blood test indicates the development of tick-borne encephalitis when leukopenia and thrombocytopenia are detected, and the amount of liver enzymes also increases.
To diagnose borreliosis, the following tests can be performed:
- Immunoassay for the content of immunoglobulins of classes M and G in the blood;
- Immunoblot - with it, species-specific proteins for Borrelia are detected in the blood. By itself, this analysis is not representative, but when carried out in parallel with an immunological study, it confirms its result;
- Polymerase chain reaction (PCR) is an addition to the previous two tests. In this case, the cerebrospinal or joint fluid is examined for the presence of bacteria. The material sampling procedure consists in puncture (puncture) of the spinal cartilage and fluid sampling. The procedure is very painful.

The results of immunoassay, as the most informative study, are deciphered as follows:
- Less than 10 U / l IgG and less than 18 U / l IgM - the result is negative. Either there is no infection, or the test was taken too early (even before the start of the immune response);
- 10-15 U/l IgG and 18-22 U/l IgM - a questionable result, but infection may develop;
- Over 15 U / l IgG and over 22 U / l IgM - the result is positive. Either the disease develops, or these are preserved antibodies after another disease - syphilis, mononucleosis and some others.
The results of the tests should be deciphered only by a doctor. He will decide on the start of treatment. If encephalitis is detected, the patient is prescribed treatment in a hospital (sometimes an intensive care unit is required), with borreliosis, depending on the stage and condition of the patient, therapy is carried out both at home and in the hospital.
Methods for early diagnosis of tick-borne infections
Given the danger of tick-borne infections, their severe consequences and the complexity of the treatment of tick-borne encephalitis, in some cases it is advisable not to wait for the onset of symptoms of the disease, but to take preventive measures immediately after a tick bite. This is true provided that the tick has bitten a person in a region with a high incidence of tick-borne encephalitis and borreliosis.
So what to do in this situation:
- Keep the tick removed from the skin (it is desirable to keep it alive, but a dead parasite will also work for analysis). The tick should be put in a jar, and next to it - a piece of cotton wool or a napkin soaked in water (so the parasite will be suitable for research longer). For useful information, see also the article What to do if bitten by a tick: help a person at home.
- Within 1-2 days, deliver the tick to the laboratory. Addresses and phone numbers of the relevant institutions can be given at any clinic (including by phone);
- Submit a tick for analysis, pay for the study and wait for the results;
- If the tick is infected with an infection, contact an infectious disease specialist with the results of the analysis.

If an unvaccinated person in a region dangerous for encephalitis is bitten by an infected tick, there is a chance that the victim will develop this disease.
It makes no sense to donate blood for analysis before the first symptoms of tick-borne encephalitis and borreliosis appear (or rather, in the first 2 weeks after the bite). There will be so few pathogens, their antigens and specific immunoglobulins that it will not be possible to reliably interpret the result of such an analysis.
On a note
There is an opinion that it makes no sense to conduct a tick test for borreliosis. This disease is successfully and quickly treated with timely therapy, and taking into account the low probability of infection even from an infected tick, there is no particular need to identify the pathogen in the body of the parasite. Thus, it makes sense to analyze a tick for borreliosis mainly for complacency.
On the prevention of tick-borne encephalitis and borreliosis
Specific prophylaxis today has been developed only for tick-borne encephalitis. People living in epidemiologically dangerous regions, or traveling here, are given vaccination, which with a probability of about 96% will protect against the development of the disease during the transmission of the pathogen from the tick. To date, this is the most effective way to prevent TE.

If a person does not have a vaccination, and he was bitten by a tick infected with a virus, it is advisable to carry out emergency prevention of tick-borne encephalitis. If the parasite was investigated quickly, and no more than 3 days have passed since the bite, such prophylaxis can prevent the development of the disease. It consists in the introduction of human serum immunoglobulin against the tick-borne encephalitis virus into the blood.Although the reliability of such prevention is not absolute, statistics show that people who have passed it get sick with tick-borne encephalitis less often than those who have not had it, and if the disease develops, it proceeds in a mild form and does not leave serious consequences.
Emergency prevention of borreliosis is not carried out: for those people who do get sick, this disease is relatively easy to cure. For this reason, even if a person has been vaccinated against tick-borne encephalitis, one should carefully monitor one's own condition after a tick bite - the vaccine does not protect against borreliosis, and therefore, with the development of the disease, it is important to recognize it in time.
The prevention of the bites themselves is also important:
- Use of clothing that prevents ticks from entering the body (pants tucked into socks, a shirt or windbreaker tucked into pants, a hood);
- Staying in nature in light-colored clothes, on which it is easy to detect ticks;

- Regular examinations of the body during a long stay in nature (for example, on a camping trip or hunting);
- Use of DEET-based repellents in combination with acaricides;
- Avoiding areas with tall grass, paths along which wild and domestic animals often move (ticks find them by smell and wait for their victims here).
Practice shows that even people who are often in nature, if these rules are followed, are almost never bitten by ticks and do not get sick with the corresponding diseases.
What threatens a tick bite: possible consequences and first aid