Tick-borne encephalitis and Lyme disease are two of the most well-known, but far from the only, diseases that ticks carry. Even if we do not take into account the diseases that these parasites infect animals, and list only those that can infect humans, we get a very impressive list.
Moreover, in different countries, the diseases carried by ticks can vary greatly, and in some places infections that, for example, Siberians have not even heard of, can annually take more lives than the same tick-borne encephalitis in Russia.
However, even on the territory of Russia, Ukraine or Kazakhstan, a tick can be infected with a very rare infection, the name of which is definitely not well-known, but which can be not only very unpleasant, but also extremely dangerous, up to a threat to human life. Therefore, it is useful to know about such tick-borne diseases, at least in order to be able to consult a doctor with the corresponding symptoms in time.
A variety of diseases, the pathogens of which are carried by ticks
All diseases associated with ticks can be divided into two large groups:
- Transmissible infections for which the tick is a carrier and the pathogens of which are parasites or symbionts of the ticks themselves;
- Acariases, the causative agents or the cause of which are precisely ticks or their metabolic products.
When they talk about diseases that ticks carry, they mean infectious diseases.For example, in Russia, the best known of these are tick-borne encephalitis caused by the corresponding virus, and Lyme disease caused by Borrelia. Tholeraemia, Crimean-Congo fever and human granulocytic anaplasmosis are recorded less frequently in the post-Soviet space - all three are bacterial infections.
Acariasis is also called, for example, scabies, which occurs due to damage to the skin with an itch that gnaws moves in it.

This is how human skin affected by scabies looks like under a microscope.
Or demodicosis - a disease widespread throughout the world associated with the colonization of hair follicles and skin glands by microscopic mites of the genus Demodex (glands). Some of these diseases can be deadly (such as tick paralysis) and are generally much more common than tick-borne infectious diseases.
However, tick infections that develop in the body after being bitten by a "wild" tick in nature are perceived by people as much more serious dangers, since cases of death or disability after their course receive more information resonance.
Therefore, by the way, ixodid (and less often - argas) ticks are considered a greater evil than microscopic ticks that cause pathologies much more often.
If we talk only about those diseases that are carried by ixodid or other large ticks that feed on human blood, then they can be divided into three groups according to the type of pathogen:
- Viral, including tick-borne encephalitis;
- Bacterial - Lyme disease, typhus, tularemia, various hemorrhagic fevers, ehrlichiosis;
- Diseases caused by protozoa.Of tick-borne infections, only babesiosis is known, including those transmitted to humans.
These diseases can develop after a single bite of an infected tick, although according to statistics, the probability of infection even from an infected individual is no more than 15-18%. Further development of any of these diseases occurs without the participation of the tick.
The most famous of these tick-borne infections are:
- Tick-borne encephalitis;
- Lyme disease (Lyme borreliosis);
- Rocky Mountain spotted fever;

One of the main signs of Rocky Mountain spotted fever infection is a maculopapular rash on the body.
- Tick-borne typhus;
- relapsing tick-borne typhus;
- Plague;
- telaremia;
- Marseille fever;
- Human granulocytic anaplasmosis.
According to the nature of the course, tick-borne paralysis is similar to transmissible tick-borne infections. This disease develops due to the action on the human body of a toxin secreted by females of several species of ixodid. Its lethality is about 6% worldwide, and ticks possessing such a toxin are also found in Eurasia, although it is mainly livestock that suffers from them, and signs of it are rarely detected in people in Europe and most of Russia. This disease occurs in the form of rapidly developing paralysis, which can lead to death due to suffocation. Usually, her symptoms quickly end immediately after the removal of the tick.
More typical, more common, and more epidemiologically significant acariasis in humans include:
- scabies;
- Ixodiosis is a painful skin reaction to ixodid tick bites. It is manifested by the appearance of redness, itching, pain, blisters at the sites of bites, and then can be supplemented by an inflammatory reaction;
- Argasosis is a disease similar to ixodiosis, but develops as a result of the bites of argas ticks. Moreover, if ixodids bite painlessly and imperceptibly, then the bites of some argasids are extremely painful. For example, the saliva of the Persian tick is toxic and bites often develop a fever, from which deaths have been reported. And shell mite stings are considered more painful than bee stings;
- Acarodermatitis;
- Demodicosis - inflammation of the sebaceous glands and hair follicles, in which the glands settle;
- Tick-borne allergy, manifested by dermatitis, rhinitis, bronchitis and sometimes can progress to bronchial asthma. The most common causative agents of it are dust mites living in apartments and houses.

Dust mites under a microscope. It lives in houses, feeding on microscopic pieces of skin, hair and other organic particles.
Ticks also cause a large number of diseases that are dangerous to pets. Among them there are both those that people do not suffer from (for example, piroplasmosis, which is very dangerous for dogs), and diseases common to humans and animals - ehrlichiosis (aka anaplasmosis), borreliosis, tick-borne paralysis. Moreover, some of them are relatively easily tolerated by animals (or animals do not suffer from them at all, but serve as their carriers and natural reservoirs), but for humans, these same diseases can be a mortal danger.
Let's take a closer look at these diseases...
Tick-borne encephalitis and its danger
Tick-borne encephalitis is one of the most famous diseases in Eurasia, the main carriers of which are ixodid ticks.It is deadly, its lethality is approximately 1.6%, and the most dangerous are the Siberian and Far Eastern forms, caused by the corresponding subtypes of the pathogen. Encephalitis in these forms has a mortality rate above 5%, while the disease of the European subtype is usually milder and very rarely fatal.
The causative agent of tick-borne encephalitis is a virus of the flavivirus family, the so-called tick-borne encephalitis virus. It is distributed throughout Eurasia from the Pacific coast to the Baltic countries, and is found only in temperate and subtropical climates, exactly where the ticks that carry it live.
Of the variety of ixodid ticks living in Europe and Asia, the tick-borne encephalitis virus is confirmed to be transmitted by 14 species from 3 different genera. However, the greatest number of cases of infection with this disease was registered after the bites of two species: a dog tick in Europe and a taiga tick in Siberia and the Far East.

Most often, infection with tick-borne encephalitis occurs from taiga and dog ticks.
Actually, it is in the organisms of these types of ticks that the virus circulates and is constantly maintained in nature. A significant reservoir of it is also wild animals, tick hosts, through which, among other things, the pathogen is transmitted from one tick to another, although this route is not the only one. Such hosts in the wild are ungulates, hares, foxes, rodents, and on pastures - including livestock.
Since ticks in the wild are active only in warm weather, human infections occur only from spring to early autumn, and the disease itself is often called spring-summer tick-borne encephalitis.
It is interesting
A person can become infected with tick-borne encephalitis after drinking unboiled milk from infected goats and cows. Such cases, although rare, are regularly recorded.
The disease itself is characterized by damage to the brain and its membranes, that is, it is a typical neuroinfection. At the end of the incubation period of 7-12 days, a person develops a fever typical of viral diseases, which disappears after 5-6 days, and then, after a short break, neurological symptoms develop, from pain in the head and muscles to impaired coordination of movements, paresis and paralysis. In severe forms, the disease is fatal.
On a note
According to statistics, after the onset of neurological symptoms, the mortality rate of tick-borne encephalitis is 22-42%, depending on the region in which the bite occurred. Most of the cases of the disease proceed without the development of such symptoms and end with the complete recovery of the bitten.
There are currently no drugs that allow you to quickly, completely and surely destroy the tick-borne encephalitis virus in the human body. Treatment of the disease is carried out with the help of gamma globulin preparations and immunostimulants based on interferon.

Interferon is the basis for drugs used in the treatment of tick-borne encephalitis.
Additionally, the patient is prescribed auxiliary means and methods of treatment that alleviate his condition and speed up recovery. Despite the fact that this technique is quite effective, it does not provide an absolutely reliable cure for the disease.
Sufficiently reliable protection against tick-borne encephalitis is considered vaccination.Actually, due to its introduction into practice in Europe, the development of drugs for the treatment of encephalitis is not being carried out, since the need for them is constantly decreasing - the population in epidemiologically dangerous areas is actively vaccinated and the relevance of tick-borne encephalitis is steadily decreasing.
Effective vaccination involves the administration of the drug three times for maximum effectiveness, but even one vaccination guarantees that encephalitis will not kill a person: after it, in extreme cases, the disease will pass in a mild form and end without consequences.
Lyme disease (tick-borne borreliosis)
Lyme disease is considered by the general public to be a kind of "smaller" version of tick-borne encephalitis, less formidable, but still unpleasant.
In reality, this disease is of a completely different nature and, apart from a symptomatic picture (and only partly) and transmission by ticks, has practically nothing to do with encephalitis.
Moreover, Lyme disease is especially insidious due to the variety of its manifestations and the fact that it can manifest itself both a week after the bite and two years later, when a person already has time to forget about the bite itself. Because of this, in many cases it is either misdiagnosed or not diagnosed at all. As a result, the patient does not receive the correct treatment, because of which he may develop chronic lesions of internal organs and joints, sometimes ending in disability or even death. Moreover, in many cases, neither the patient nor even the doctors treating him suspect that the cause of his serious condition and the progression of the disease is precisely borreliosis.

One of the complications of untreated borreliosis can be neuritis of the facial nerve.
In addition, according to world statistics, Lyme disease is the most common tick-borne disease in the Northern Hemisphere. In terms of the number of people infected and constantly infected by it, it is ahead of even tick-borne encephalitis.
Lyme disease is caused by bacteria of the genus Borrelia, and in different countries - by different types of them. These pathogens in natural conditions infect various wild animals - goats, sheep, foxes, wolves, hares, rodents, roe deer and deer. They are also sources of infection for ticks, although the ability of the pathogen to be transmitted between the female and tick larvae transovarially, that is, through eggs, has been proven. When infected hosts are bitten by ticks, Borrelia enter their digestive tract with blood, spread in the tissues of the parasite, and eventually penetrate into the salivary glands. If after that the tick bites a person, then Borrelia will penetrate into the tissue at the site of the bite with saliva.
The disease is obligately transmissible, that is, it is impossible to catch it otherwise than from a tick.
After infection of the body, bacteria quickly spread to different tissues and organs. During their vital activity, they release toxins that lead to the development of general symptoms of the disease (fever with fever, malaise, vomiting) and local inflammatory reactions. A variety of organs can be affected, and often the clinical picture of borreliosis resembles the clinical manifestations of dozens of other diseases.
The main diagnostic sign of Lyme disease is erythema migrans in the form of a spreading red ring on the skin around the bite site. It clearly indicates an infection. However, in many cases of the disease, such erythema does not appear at all.
Another difficulty in diagnosing borreliosis is that its incubation period can last from 5-6 days to several months and even up to 2 years. Of course, six months after a tick bite, few people will remember about it, and the typical symptoms of borreliosis in the middle of winter can be interpreted incorrectly.
Finally, Borrelia themselves are very difficult to identify in the body for accurate instrumental diagnosis. They can be found in different tissues in different forms, including in the form of spores, they usually inhabit tissues in very small quantities and are generally very small in size, and therefore it is rarely possible to detect them.
On the other hand, treatment of borreliosis in the early stages is not very difficult. Borrelia are sensitive to inexpensive antibiotics - doxycycline, tetracycline, amoxicillin. Standard courses of taking these funds can completely cure the disease.

Drugs to cure borreliosis in the initial stages of the disease.
At the same time, advanced borreliosis in the later stages is not always treatable and can lead to arthritis, acrodermatitis, and focal scleroderma. The disease in pregnant women can lead to infection of the fetus and death of the newborn. Therefore, after a tick bite, it is necessary to consult a doctor if symptoms of the disease appear, or if such symptoms do not appear, after 2-3 months, take a blood test to detect antibodies to Borrelia. Further actions will already be indicated by the infectious disease specialist.
Rocky Mountain Spotted Fever
Rocky Mountain spotted fever is a disease endemic to the New World, that is, all its cases have been recorded only in North and South America, most often in the United States, less often in Brazil, Colombia and Canada.It is caused by the rickettsia species Rickettsia rickettsii, the natural reservoir of which is wild animals, and the carriers are ixodid ticks.
It is interesting
The disease got its name because of the place of registration of the first epidemic in the state of Montana in the foothills of the Rocky Mountains.
The disease is extremely dangerous for humans. Even with a favorable course, it causes the appearance of numerous hemorrhages, in places of which skin necrosis with gangrene can develop. The acute phase is very difficult for a patient with high fever, bloody vomiting and diarrhea.
Before the advent of antibiotics, Rocky Mountain fever had a fatality rate of over 30%. Today, it is successfully treated with doxycycline, but even with modern methods and means, the lethality of the disease is 5.2% (every twentieth sick person dies), and many seriously ill people lose their hearing.
Tick-borne typhus
This disease is relatively rare and today only occurs in eastern Siberia and the Russian Far East. It manifests itself with fever and the appearance of a profuse rash in the form of small papules all over the body. Usually, such signs of the disease appear 4-5 days after a tick bite.

The first sign of tick-borne typhus is fever, chills, and fever.
The prognosis is favorable, and deaths are extremely rare. Without the use of antibiotics, the disease lasts 2-3 weeks and gradually ends with a complete recovery. When taking tetracycline antibiotics for 2-3 days of treatment, the patient's condition returns to normal.
Interestingly, tick-borne typhus, as an obligate transmissible disease, is not transmitted from person to person except through ticks. Because the likelihood of two people being bitten by the same tick is small, the sick person is not considered contagious.Unless, of course, it is precisely established that he has typhus.
relapsing tick fever
Despite the similar names and external similarity of symptoms with the previous disease, tick-borne relapsing fever is caused by a completely different pathogen. If typhus is caused by rickettsia, then relapsing fever is caused by borrelia and is etiologically closer to Lyme disease.
At the same time, the causative agent of tick-borne relapsing fever is a completely different type of borrelia than the one that causes Lyme disease. If Lyme borreliosis is caused by Borrelia burgdorferi, then the causative agent of relapsing fever is Borrelia Obermeyer (Borrelia recurrentis). Both of them belong to spirochetes, but the diseases they cause differ significantly.

It looks like the bacterium Borrelia recurrentis, which is the causative agent of relapsing tick-borne typhus.
Relapsing tick-borne typhus is carried by argas, not ixodid ticks. Its most significant carriers are the Persian and settlement ticks, which are widespread in Central Asia. They parasitize on birds, rodents, domestic animals, and when settling in a person’s housing, they bite him too, and their bites themselves are very unpleasant and cause severe painful itching. After being bitten by a tick infected with Borrelia, a person can develop typhus.
On a note
The same types of ticks carry the plague in those areas where wild populations of rodents - ground squirrels, jerboas, gerbils - are infected with it. Therefore, when visiting such places, and even more so if you need to work in them, special measures are required to prevent argasid bites.
The disease got its name because it usually proceeds in the form of two attacks with fever and rashes all over the body, that is, after a temporary relief, the disease seems to return.The interval between attacks is 5-8 days.
Tick-borne relapsing fever today continues to be a dangerous disease for humans, especially in countries with poor nutrition and low levels of health care. People who eat well and nutritiously usually recover after two attacks of the disease, relatively rarely they develop complications in their eyesight and heart. In countries with low levels of health care and in people infected with HIV, the mortality rate of tick-borne relapsing fever can be as high as 80-90%.
In general, tick-borne relapsing fever is effectively treated with tetracyclines, ampicillin, and levomycetin. With timely competent therapy, the risk of complications and even more death is very small.
Marseille fever
This disease is very similar to Rocky Mountain spotted fever. It is also a rickettsiosis, caused by Rickettsia conorii, and clinically resembles a milder version of Rocky Mountain fever.
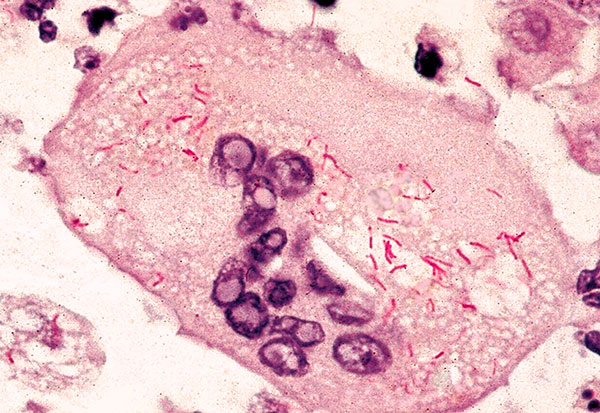
Rickettsia conorii bacteria in a blood smear.
On a note
Previously, Marseilles fever was called Tunisian endemic typhus - outwardly, the rashes with it are similar to typhoid ones, and the first description of this disease was made in Tunisia.
The natural reservoir of Marseilles fever is various wild animals, mainly canines. Its main carrier is the dog tick. Remarkably, in Europe it is not recorded in the entire habitat of this tick, but only in warm regions around the Mediterranean and Black Seas. Outside of Europe, Marseilles fever is widespread in India, Southeast Africa and Central Asia.
The disease is relatively severe, but very rarely accompanied by dangerous consequences. Most patients recover with the formation of stable lifelong immunity, which is also effective against other rickettsiosis. For example, a person who has recovered from Marseilles fever will no longer be infected with Rocky Mountain spotted fever.
Marseilles fever is relatively easily treated with tetracycline antibiotics. After the start of their intake, the person's condition rapidly returns to normal, and on the second or third day the fever ends, although spots and rashes remain on the skin for some time.
Hemorrhagic fever
The name "hemorrhagic fever" refers to several diseases caused by different pathogens, but proceeding with approximately similar symptoms: after a severe fever, the patient develops numerous hemorrhages on the skin and mucous membranes. These hemorrhages may appear as pimples, rashes, large patches, or bruises.

A sign of hemorrhagic fever is hemorrhages on the skin.
Intoxication of the body leads to vomiting, diarrhea, abdominal pain, in women - to uterine bleeding. Normally, after 10-12 days, the fever weakens, but even before a month the patient can be very weakened.
In rare cases, patients with hemorrhagic fever develop sepsis, leading to death. The overall lethality of the disease is 4-5%.
All hemorrhagic fevers are caused by viruses. At the same time, there are not so many of them carried by ticks:
- Crimean-Congo fever, notable in that it was described as two different diseases from the Crimea and from Central Africa, and then the researchers found that the causative agent there and there is the same virus;
- Omsk hemorrhagic fever, widespread in the forest-steppe areas of the Omsk, Orenburg, Novosibirsk, Tyumen and Kurgan regions.
On average, 50-100 cases of Crimean-Congo fever and up to 200 cases of Omsk hemorrhagic fever are reported annually in Russia. Both diseases are quite difficult, but in most cases they end in complete recovery. Etiotropic treatment does not exist today, patients are prescribed medications to relieve symptoms and general restorative therapy.
Tularemia
Tularemia is a disease that is widespread throughout the northern hemisphere of the planet and mainly affects wild mammals, mainly rodents. It can occur in various forms, including the so-called "bubonic" with the appearance of characteristic blister-like formations on the skin. In this form, it is also called "little bubonic plague", with the prefix "little" being used to indicate that tularemia is less dangerous than plague.
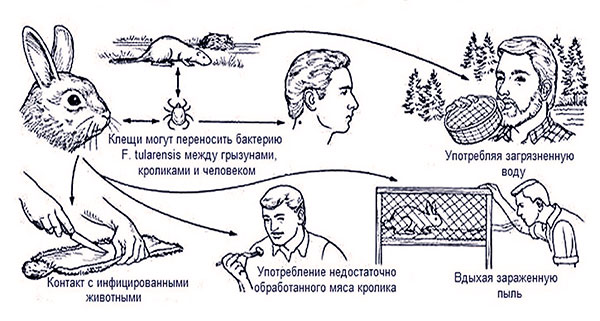
Ways of infection with tularemia.
It is interesting
Tularemia was discovered precisely during the study of natural foci of plague, when obviously infected ground squirrels and voles were examined, but the plague pathogen was not identified in them. A closer study made it possible to detect in them a microorganism unknown at that time, which was subsequently well studied, was named Francisella tularensis and described precisely as the causative agent of tularemia.
In Russia, tularemia occurs in all regions, and in some places outbreaks of the disease occur regularly. The most massive of them in this century occurred in 2005, when the disease was diagnosed in several hundred people. It is associated with the abolition of mass vaccination of the population against tularemia.
The disease can occur in different forms, which greatly complicates its diagnosis. Anginal, bubonic, intestinal, pulmonary, conjunctival, generalized (the most dangerous) and other forms of the disease are described. With any course of a patient with tularemia, it is necessary to hospitalize with isolation from other patients. Treatment is with antibiotics.
Tularemia is not an obligate transmissible disease. It can be transmitted by airborne droplets and contact, through contaminated water and food, as well as through blood-sucking insects and ticks. Such a variety of ways of its transmission is associated with the highest resistance of the pathogen to adverse environmental factors - Francisella survives for months in ice and frozen meat, in the skins of dead animals, in water, soil and food. Therefore, in general, the probability of infection with it from ticks is not so high - more often people become infected in other ways.
tick paralysis
This disease belongs to acariasis because it is not caused by an infectious agent. Its cause is a toxin that is contained in the saliva of some types of ixodid ticks and can cause paresis and paralysis in humans and animals.
The Australian paralytic tick Ixodes holocyclus is best known for this ability - several dozen people die from its bites every year in Australia. However, paralyzing mites are distributed throughout the world and are found, including in Russia.

The bite of the Australian paralytic tick can be fatal.
It is known that paralysis can develop only after the bites of adult female ticks, and only those that are on the body for more than 48 hours.Apparently, only at this stage of feeding they begin to produce a toxin.
If such a female is removed at the first signs of illness, all symptoms usually subside quickly and the person recovers. Very rarely, the disease can progress after the removal of the tick.
Actually, the only sufficiently effective way to treat tick paralysis is to remove the tick and therapy aimed at restoring the activity of the affected muscles.
What diseases do ticks not tolerate?
Contrary to popular myths, ticks do not carry many infectious diseases that, at first glance, could be transmitted with the blood they pumped.
For example, ticks do not carry HIV and cannot infect humans with AIDS, since the human immunodeficiency virus does not survive in the tick's body and is not able to penetrate the salivary glands.
Also, when bitten by a tick, you can not get infected:
- Hepatitis - neither hepatitis B nor hepatitis C;
- syphilis;
- We deprive or any fungal infections.
In general, almost all diseases (with the possible exception of tularemia) transmitted by ticks to humans are not transferred between people without the participation of ticks. Therefore, the opposite is also true: if the disease can be transmitted in a non-transmissible way, then ticks do not tolerate it.
When and how does tick-borne infection occur?
All tick-borne infections are transmitted to humans only by tick bites. If the tick only crawled over the skin, but did not bite, you can be sure that it definitely did not infect a person with anything.
It is believed that the likelihood of infection increases as the tick sucks blood and increases in size. That is, the longer it bites, the more likely it is to become infected.

The longer the tick drinks blood, the higher the chance of contracting tick infections.
There are no specific deadlines before the expiration of which we can talk about a “safe” bite. Claims that if the tick is removed in the first 2, or 4, or 24 hours after biting, then the disease will not develop, are nothing more than assumptions. Theoretically, infection can occur at the very first injection of saliva by the parasite into the wound in the skin, that is, already in the first seconds of the bite.
In general, the likelihood of something getting infected from a single tick bite is small. For example, in a region epidemiologically dangerous for tick-borne encephalitis, the probability of infection from one tick is approximately 0.2%. That is, out of 1000 bites, 2-3 lead to infection. Even if a uniquely infectious tick bites, in which the pathogen is then detected in the body, the probability of infection from it is approximately 15%. At the same time, the percentage of ticks infected with this infection, even in heavily tick-infested areas, does not exceed 14-16%.
The statistics for Lyme borreliosis are approximately the same, and infection with other tick-borne infections is even less likely.
Cases of infection with tick-borne encephalitis have been confirmed by drinking fresh milk from goats and cows infected with the virus. Similarly, tularemia is transmitted in many ways, but it is not a typical tick-borne infection.
Presumably, an infection from a tick can be contracted if you accidentally crush it in your hand, and there are fresh scratches or wounds on the hand itself - the pathogen can enter the blood through the wound. However, the likelihood of such an infection is extremely low. At a minimum, crushing a tick in your hand is very difficult due to the high strength of its body integuments. And in order for this to coincide in time with the presence of open scratches on the palm or fingers, you need to try very hard.As a result, no cases have been reported in which tick-borne infection would be transmitted in this way.
All this means that the best way not to get infected with anything from ticks is not to let the parasites bite you. And for complete reliability, it is recommended to be vaccinated against tick-borne encephalitis and tularemia. With such protection, you can confidently go out into nature even in the most densely populated places with ticks and not be afraid for your health.
About diseases that are carried by ticks in questions and answers



