A tick bite, especially if it lasts more than 10-15 minutes, often causes rather unpleasant consequences for a person. Sometimes even a shorter-term suction of the parasite leads to undesirable manifestations, but in general, it is 10 minutes after the puncture of the skin that the tick manages to inject its saliva with all its components into the subcutaneous tissue and pump the first portion of blood.
All the consequences of a bite can be divided into several groups according to the degree of their danger to humans:
- Infectious diseases, the pathogens of which are transmitted with the saliva of the tick during bloodsucking. Some of these diseases are deadly, killing several hundred people in Russia and thousands of people around the world every year. This group also includes tick-borne paralysis, which is not an infectious disease, but is also deadly;
- Diseases that are prone to transition into a chronic form, often with disability and a significant deterioration in the quality of life of a bitten person;
- Consequences that do not pose a serious threat and relatively quickly passing (in 2-3 days), but manifested by unpleasant symptoms.
In the vast majority of cases, tick bites are accompanied by the consequences of precisely the third group - a person needs to endure them for a couple of days, and then they pass without a trace. In less than 1% of bite cases, the consequences of the first two groups develop, which, in fact, provided ticks with gloomy glory.Let's look at all these consequences and see how to identify them at the stage when they can be eliminated relatively quickly.
Deadly consequences of tick bites
The most infamous disease in Eurasia transmitted by the bite of ixodid ticks is tick-borne encephalitis. The virus-causative agent in the first stage of the disease affects macrophage cells, as well as the liver, spleen and lymph nodes. Having multiplied here in sufficient quantities, it penetrates the cells of the spinal cord and brain and actively multiplies there. In the absence of treatment at this stage, irreversible neurological and mental disorders develop, which in severe situations end in death.
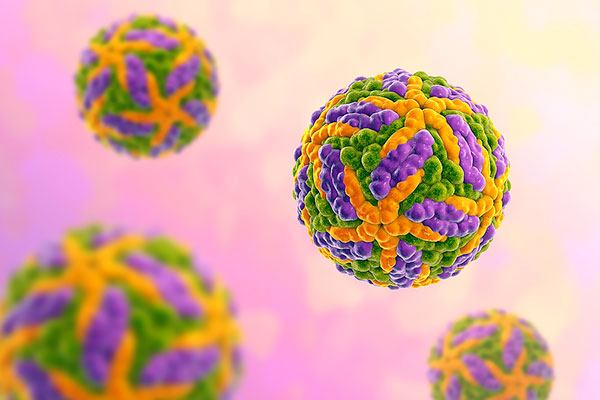
The tick-borne encephalitis virus primarily affects the cells of the immune system.
It must be recognized that in most cases, even without treatment, tick-borne encephalitis ends with a complete recovery of the bitten. According to statistics, a disease caused by a virus of the European subtype has a lethality of 1-2%, and caused by the Siberian and Far Eastern subtypes - 20-25%. Irreversible consequences on the part of the nervous system and psyche develop on average for both types in 10-15% of the diseased, but surviving people.
Tick-borne encephalitis itself occurs in several forms, and only some of them are manifested by symptoms with a standard fever (the temperature rises, malaise develops, the person feels nausea, loss of strength, drowsiness), while others develop more pronounced and severe symptoms.
It is very characteristic to divide the entire period of the course of the disease into two stages with a break of several days between them.In the first stage, the disease proceeds like a typical viral infection, with fever, headaches, malaise, but nothing more. Then the patient's condition returns to normal, he may believe that he has already recovered, but after a few days he suddenly becomes ill, neurological symptoms appear, up to fainting and paralysis.
The disease caused by the European subtype often occurs either in this form, or with the presence of only the first stage, without the involvement of the nervous system in pathogenesis. When infected with a virus of the Far Eastern (more dangerous) subtype, there is often no break between stages, and the patient's condition is steadily and rapidly deteriorating.

The condition of a person affected by tick-borne encephalitis of the Far Eastern subtype is rapidly deteriorating.
According to statistics, death occurs on average 5-7 days after the onset of neurological symptoms. If intensive treatment is started on time, a complete recovery is possible, but sometimes even after treatment there are consequences: paralysis, paresis, epileptic seizures, mental disorders. Here the statistics are inexorable: in patients who develop neurological symptoms during the course of the disease, the probability of maintaining irreversible consequences is approximately 45%.
On a note
It is not known how encephalitis infection affects the fetus during pregnancy of a bitten woman. There is no relevant documentary evidence, but given that the disease is deadly for the bitten person, the seriousness of its consequences during pregnancy is not even called into question.
And one more important detail: today, etiotropic therapy has not been developed against tick-borne encephalitis.Simply put, in the arsenal of doctors there are no drugs that are guaranteed to cure the patient. But for the prevention of the disease, a highly effective vaccine has been developed, the correct use of which guarantees that the disease will not develop after a bite of an encephalitis tick.
Another deadly disease transmitted by tick bites is Lyme borreliosis. Its causative agents are several types of spirochetes, united in the Borrelia burgdorferi group. Once in the body, they affect the joints and heart, sometimes the nervous system. If untreated, the infection progresses and becomes chronic, which can be fatal.
Lyme borreliosis is considered the most common tick-borne disease in the Northern Hemisphere. It affects not only people, but also domestic and wild animals. At the same time, it is considered less dangerous than encephalitis, due to lower mortality and due to the fact that, with timely diagnosis, it can be reliably cured with antibiotics.
But, in fact, the diagnosis of borreliosis is often very difficult. In the standard case, the disease manifests itself as a very characteristic annular migratory erythema (redness in the form of a ring) around the bite site, but quite often such erythema does not appear at all, and sometimes the incubation period of the disease drags on for months and even years, after which the bitten person does not even remember, that he was bitten by a tick.

The appearance of annular erythema at the site of a tick bite is a clear sign of infection with borreliosis.
In addition, at those stages at which the treatment of borreliosis is most effective, it is very difficult to diagnose it using reliable methods, since the number of spirochetes in the body is very small, and antibodies to them are not yet produced in sufficient quantities for detection.
It is these difficulties in diagnosis that lead to the emergence of a large number of cases of neglected and intractable disease, which causes a high risk of borreliosis.
Also, many fevers, the pathogens of which are carried by ticks, are still deadly. The most famous of them are:
- Rocky Mountain spotted fever - its lethality today is about 5%, but before the invention of antibiotics, it reached 30%. Distributed in the USA, Canada and countries of Central America, caused by rickettsiae and carried by ticks common to the western USA;
- Omsk hemorrhagic fever with a mortality rate of 1-5%. Distributed in Omsk, Novosibirsk, Kurgan, Tyumen and Orenburg regions. It is caused by a virus, which is why its treatment is carried out only by means of symptomatic and supportive therapy;
- Crimean-Congo hemorrhagic fever, also of viral etiology, with mortality in the range of 20-22%.
With spotted fever of the Rocky Mountains, the Marseilles fever, common in the Mediterranean, in the Crimea, as well as in the south of Ukraine and in the Transcaucasus, is also similar in etiology. It is also caused by rickettsiae and after its transfer, a person develops lifelong immunity both to it and to other rickettsiosis, including Rocky Mountain fever. But, despite the relatively severe course, this disease rarely leads to death.

Marseilles fever is manifested by a vesicular rash on the skin.
Finally, tick-borne paralysis is a mortal danger to humans. This disease develops due to the ingestion of tick-borne toxin, which is secreted by adult females of some types of ticks on the 3rd-4th day of bloodsucking (on average, a bite lasts from 5 to 7 days). The best-known such species is the Australian paralytic tick, whose bites kill several dozen people and a large number of livestock in Australia every year. But also on the territory of Russia, in Ukraine and in Western Europe, there are several types of ticks, the females of which secrete such a toxin.

Ticks can release toxins that cause paralysis.
The main distinguishing feature of such paralysis is the absence of generalized symptoms. A person does not have a fever, weakness or malaise does not appear. It’s just that at some point he feels that he is losing control over one or another limb, or he develops a tremor or paresis. These symptoms progress rapidly until asphyxia develops and the person dies of suffocation.
In most cases, to treat tick paralysis, it is enough to find and quickly remove the attached tick. After that, within a few hours, the condition of the victim returns to normal, although in rare cases (or with a reaction at a late stage), urgent hospitalization of the bitten is required. At the same time, official data on mortality from tick-borne paralysis is about 12% of the number of diagnosed cases.
Diseases transmitted by ticks and fraught with chronic forms
In the chronic form, Lyme disease and tick-borne encephalitis can occur.
For borreliosis, the chronic form is, if not the norm, then not a rare case.If the patient has not received treatment and the disease has not ended on its own, with a high probability it will turn into a chronic form.
In cases where borreliosis ends fatally, it is the chronic form of the disease that precedes death. With it, various autoimmune reactions develop, damage to the heart, joints and nervous system occurs, and secondary syndromes appear. Many of them significantly reduce the quality of life of the patient, but are not treatable. It is the autoimmune consequences, coupled with the intracellular localization of the main part of Borrelia in the body, that make the disease at this stage practically incurable.

The chronic form of borreliosis leads to damage to the joints and nervous system with the manifestation of secondary symptoms.
On a note
Chronic Lyme disease can occur in both continuous and relapsing forms.
Tick-borne encephalitis in a chronic form is rare, reliably established clinical cases of such a course of the disease are rare. Pathogenetically, in this case, viral particles are constantly produced by the affected nerve cells, but they are destroyed by the immune system, and relapses occur from time to time precisely against the background of a weakened immune system. In this case, the severity of relapses can both progress and decrease from one episode to another. In the first case, a fatal outcome of one of the subsequent relapses is possible.
Non-dangerous, but rather unpleasant manifestations
The most common, rather unpleasant, but low-dangerous consequences of tick bites are local reactions of the skin and underlying tissues to the bite itself and, to a large extent, to the removal of the tick.
The fact is that when bloodsucking, the tick to some extent damages not only the skin, piercing it with its hypostome, but also the subcutaneous tissue under it. With such damage, destroyed cells appear here, the contents of which flow into the intercellular space and signal the body about the injury. Cells of the immune system flock here, an inflammatory exudate accumulates, the task of which is to eliminate the consequences of trauma and destroy infectious agents that could get here and which the immune system is able to recognize. However, this does not happen due to the fact that together with the blood, the tick sucks out this exudate - it also serves as food for the parasite.

Model of a tick in the process of piercing human skin.
As a result of this, redness and inflammation form at the site of tick attachment, which constantly progresses as blood is sucked. This, however, does not happen very quickly. And when the tick is removed (or it detaches itself), all inflammatory processes at the site of the bite begin to proceed normally. As a result, a red bump forms here, quite hard, sometimes very painful and almost always itchy. Its dimensions are from 1 to 2 cm in diameter, it can rise above the skin by 2-3 mm, in the center of it the skin puncture point is clearly visible.
Very rarely, blood flows from the bump after the removal of the tick. If this happens, it is enough to apply a cotton swab dipped in alcohol to it for a few minutes.
If the bite itches or hurts, it should be lubricated with any anesthetic ointment. This is especially important to do if the tick has bitten the child so that he does not comb the bite and does not bring the infection into the wound.
If there is no bleeding and itching (or if the itching is tolerable), nothing needs to be done with the wound at the site of the bite. After a few hours, the bump will stop itching, the redness will disappear the next day, and the bump itself will resolve in another day or two.

The inflammatory process at the site of the tick bite should pass in a few days.
Sometimes an infection is introduced into the wound at the site of the bite after the removal of the tick. This can happen for three reasons:
- If the itchy bump is constantly scratched, an infection from the fingers can get into the scratch on it;
- In the wound at the site of the bite, the head of the tick remained, if only the body came off when it was removed;
- When the tick was removed, it was crushed and the infection from its body got into the wound (this is unlikely, but it is indicated as a means of transmission of some tick-borne infections).
If the head of the tick remains at the site of the bite (it looks like a noticeable round splinter), it must be removed with cosmetic tweezers, like a simple splinter. The place of suppuration should subsequently be pierced with a sterile needle, squeeze out the pus, and smear the place of suppuration with alcohol.
Sometimes people who are bitten develop allergies. It is manifested by redness near the site of tick suction, in some cases - urticaria and Quincke's edema. Isolated cases of anaphylactic shock with a fatal outcome in children bitten by ticks are known, but they are rather an exception to the rule.

There are cases when a person bitten by a tick begins an allergic reaction.
Be that as it may, if symptoms of a severe allergy appear (usually already with hives), a person should be given any antihistamine and taken to the hospital as soon as possible. If the bitten person is allergic, he should have a suitable remedy with him.
In many cases, there are no consequences at all after a tick bite. This is especially true for situations where the parasite has just pierced the skin, but has not yet begun to suck blood and was pulled out. If you pull it, it can hardly come off the skin, since its hypostome is already fixed, but due to the absence of damage to the subcutaneous tissue, no pathological reactions occur here and inflammation with a lump does not appear.
On a note
Of course, if the tick only crawled through the skin and did not have time to pierce it and stick, there will be no consequences for a person (except, perhaps, for fear in the most impressionable people).

If the tick did not have time to stick, then there will be no negative consequences for the person.
In any case, if after a bite the swelling persists for too long, the pain does not go away, and even more so generalized symptoms develop, the bitten person should be shown to the doctor and the date of the bite reported. Not always such symptoms are associated with the bite itself, but the doctor should be aware of it.
By the way, the psychological consequences of tick bites cannot be discounted - many people are terribly afraid of these parasites, and after a single bite they may be afraid to go to nature. If the bitten person has such acarophobia, it is useful for him not to say at all that he has a tick, but to divert his attention, take hold of the tick with his fingers so that the parasite is not visible, and pull it out, saying that it is a splinter. If a tick has bitten in the head or behind the back, this is especially easy to do without scaring an impressionable person. Since with a high probability such a bite should pass without consequences, it is not worth worrying about the fact that a person does not know about it.Just in case, you can remember the date of the incident, so that if complications develop, tell the doctor already during the examination.
The likelihood of complications from tick bites
A complication after a tick bite can be considered any consequence that goes beyond the simple healing of the wound at the site of the bite. Any suppuration, severe throbbing and long-lasting pain, and even more so generalized reactions, are just complications that usually require certain specific measures.

If an inflammatory process begins to develop at the site of a tick bite, an urgent need to see a doctor.
In general, the incidence of such complications is not so great. For example:
- Allergy to components of tick saliva develops no more than in 3 cases out of a thousand bites, and most of the allergic reactions are a minor rash near the bite site. Urticaria and even more so anaphylaxis develop in isolated cases for tens of thousands of bites;
- The frequency of infection with tick-borne encephalitis in regions with a high epidemiological danger for this disease is approximately 0.24% - 24 cases of infection per 1000 registered bites. In fact, it may be lower due to the fact that only a fraction of those bites that actually occur are recorded, with almost total registration of cases of infection with tick-borne encephalitis;
- The percentage of people who became infected with borreliosis after a tick bite from all those who went to a medical institution is about 1.4%.Here the situation is similar to that for tick-borne encephalitis: in reality, significantly fewer bites are recorded than actually occur, so the proportion of those infected will also be much smaller.
There are no data on the probability of infection with various fevers (including those of a rickettsial nature) due to the same complexity of taking into account the true number of tick bites. Be that as it may, this probability is below 1%.

This is what a rash looks like on the arm of a child infected with Rocky Mountain fever.
All this means that in most cases, tick bites end without complications and the development of dangerous conditions. Moreover, even in an epidemiologically dangerous region (for example, in Siberia), tick bite can pass without consequences, and in most cases this happens. Even if a tick bites, infected, for example, with the tick-borne encephalitis virus, the probability of infection in an unvaccinated person is no more than 15%.
However, this does not mean that no precautions need to be taken when in a tick-infested area.
Signs of the onset of complications
Most of the really dangerous consequences of tick bites are manifested by generalized symptoms. Most often it is:
- Elevated temperature - from 37 to 40 °;
- Malaise, weakness;
- Muscle aches;
- Chills;
- Nausea and vomiting.
Such a typical febrile symptom complex is characteristic of tick-borne encephalitis, borreliosis, and various fevers.
More specific signals indicating a dangerous state of the body:
- Rashes on the body, with characteristic flat blisters, quickly spreading over the skin and merging into large spots - a sign of an allergic reaction;
- Paresis, impaired coordination of movements, weakness in the limbs, paralysis - a sign of either tick-borne encephalitis (if these symptoms occur against the background of fever or after it), or tick-borne paralysis (if there is no fever);
- Fainting, clouding in the eyes, drowsiness are also signs of tick-borne encephalitis;
- Erythema migrans is a spot around the bite site, gradually turning into a ring due to an increase in diameter and lightening of the skin near the bite itself. This is a clear sign of borreliosis.

An annular red spot around the site of a tick bite indicates an infection with Borrelia.
With any of these signs, as well as with a febrile syndrome that develops during the standard incubation period for tick-borne infections, you should immediately consult a doctor.
Incubation period for infection
The incubation period of tick-borne infections varies greatly both depending on the disease and in different situations in the same infection. Often this makes it difficult to diagnose diseases.
The first symptoms of tick-borne encephalitis after infection of the body appear 7-12 days after the tick bite. Moreover, fever develops first, and only then, after 5-9 days (sometimes with a pause of 2-3 days, during which the patient feels relieved), neurological symptoms appear.
Approximately the same duration has an incubation period for Lyme disease - 1-2 weeks. The only difference lies in the fact that in about 10-12% of cases with this disease, the incubation period can stretch up to several months, or it can take 2-3 days. This means that even a few years after the bite, the disease can manifest itself, when even the bitten one does not remember about the bite itself.
Hemorrhagic fevers develop in about 3-8 days. Omsk hemorrhagic fever has the shortest incubation period - often the first symptoms of the disease appear already 2 days after the bite.
On a note
It is not uncommon for the disease to begin even before the tick detaches from the body, if the person himself has not noticed it before. Infectionists regularly have situations when a person comes to them who has a fever, who is sick and chills, the doctor examines the body and finds a parasite that has attached and greatly increased in size.

Sometimes a sucking tick is found only at a doctor's appointment.
There is practically no incubation period for tick paralysis due to the characteristics of this disease - it develops while the tick itself continues to suck blood, that is, during the bite itself.
As a rule, the symptoms of allergies are growing at about the same rate. Moreover, sometimes it begins to manifest itself already in the first hours of tick attachment, when its saliva with antigens is distributed in sufficient quantities throughout the body.
Be that as it may, the symptoms of infectious diseases never develop immediately after a bite. Therefore, if after a tick bite a person develops a high or low temperature, weakness, diarrhea or vomiting, they have practically nothing to do with the bite itself. It often happens that after a long stay in nature, especially after a picnic with barbecue and alcohol, a person may have digestive disorders, or after a long stay in the sun he has a heat stroke with such symptoms, but he associates them with a tick bite that occurred on the same day.This is a mistake - immediately after a tick bite, only a rash may appear, as a sign of an allergy.
In all cases, when characteristic signs of the disease appear within a few weeks after a tick bite, you should immediately consult a doctor. No initiative is allowed here, given the mortal danger of some tick-borne infections. And after the tick bite itself, for at least two weeks, you need to monitor the condition of the bitten person in order to respond in time to signs of developing complications.
How to reduce the likelihood of dangerous consequences of tick bites
The most reliable way to protect yourself from the consequences of tick bites is to prevent ticks from biting you, or at least reduce the likelihood and frequency of such bites. For this you need:
- Wear outdoor clothing in the summer that covers your legs, body and arms. Moreover, trousers for such clothes should be tucked into socks, and a shirt or jacket - into trousers. It is desirable that such clothes be plain and light - this will facilitate the detection of ticks that have fallen on it, but have not yet had time to crawl to areas with open skin;
- If it is impossible to wear anti-mite clothing (for example, on a very hot day), use DEET-based repellents;
- Carry out self-examinations and mutual examinations of the body several times a day and remove the detected ticks from yourself or from your comrades;
- Remove stuck ticks immediately after detection, in no case should you take a bitten person with a tick in the skin to the emergency room and do not go with a tick to buy a tick;
- When staying in nature, avoid places with tall grass and paths trodden by animals - ticks usually accumulate in masses here.

In order to avoid tick bites in nature, it is necessary to wear clothing that covers all parts of the body as much as possible.
The main danger of tick bites - tick-borne encephalitis - can be avoided by getting vaccinated. It is very effective and, if carried out correctly, ensures that the disease in humans does not develop even if the pathogen is transmitted from the tick. And even if not done in full (one injection instead of three), it will prevent the development of a severe form of encephalitis and protect against the mortal danger of this disease. When planning a trip to a region with a high epidemiological risk of tick-borne encephalitis, such a vaccination is a must.
However, it is worth remembering that such a vaccination does not reduce the risk of developing other consequences of tick bites (Omsk hemorrhagic fever may be an exception to some extent), therefore, even if a person is vaccinated, when entering a ticked area, one should not forget about the rules of protection against bites of these parasites.
What are dangerous ixodid ticks and the consequences of their bites
Informative about the signs of tick-borne borreliosis